Introduction to GERD (Gastroesophageal Reflux Disease)
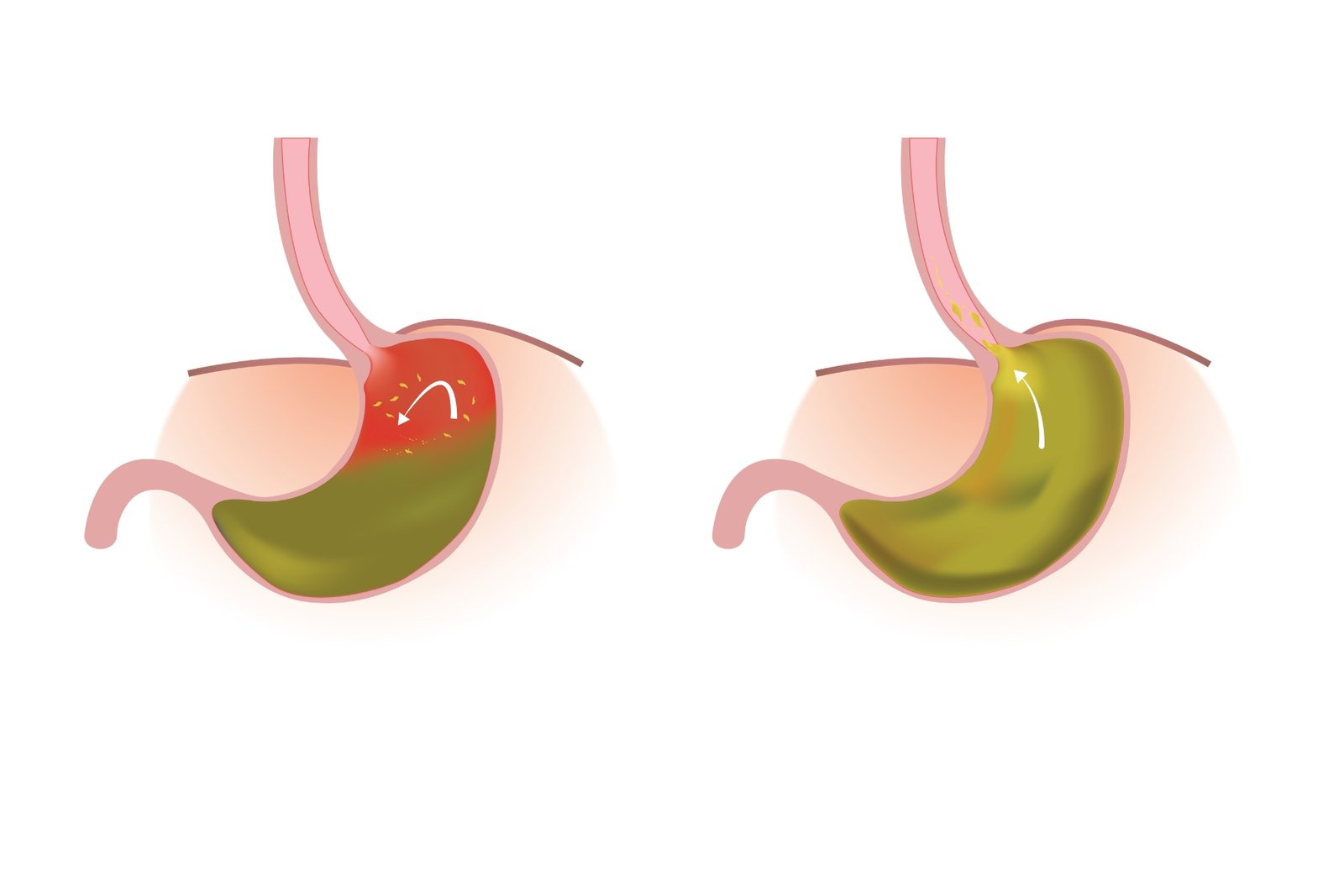
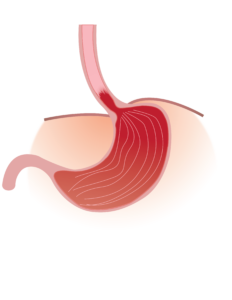
Swallowed food should move in one direction from the esophagus into the stomach and intestine distally. Digestion of food starts in the stomach; acid produced by my stomach has an important role in the digestion of food. The natural movement of stomach contents including acid and food is intended to move smoothly from the stomach into the intestine. However, this harmony is disrupted in the presence of acid reflux, a condition where stomach acid flows in the reverse direction, moving into the esophagus (food pipe) and sometimes even reaching the throat. This reversal triggers a spectrum of symptoms, including heartburn, regurgitation, chest pain, inflammation, and ulceration of the oesophagal lining.
What is GERD?
Gastroesophageal reflux disease (GERD) occurs when stomach acid flows back into the esophagus also known as food pipe. The esophagus is a conduit-like organ meant for the transfer of food from the oral cavity into the stomach. The lower esophageal sphincter a valve between the esophagus and the stomach, protects against the reflux of acid or stomach back into the stomach. Weakness of the lower esophageal sphincter leads to weakening of this barrier eventually leading to reflux. Although occasional acid reflux is common and experienced by many individuals, the diagnosis of GERD is established when this reflux becomes a regular occurrence over time, resulting in enduring symptoms and potential complications.
Esophagus is virtually a straight tube connecting the throat to the stomach. It lacks the protective lining against the acid, which is inherently present in the stomach. The stomach produces acid for digestion but is protected against the same, by virtue of a protective lining with columnar epithelium which produces mucus and other protective molecules against injury by acid present in the lumen of the stomach. When stomach acid flows back into the esophagus, an environment that is ill-equipped to handle such an acidic environment, causes inflammation and ulceration.
Differentiating GERD from Acid Reflux?
Many people have occasional acid reflux, which can be triggered by factors like specific foods, lying down after eating, physiological conditions like pregnancy, or lifestyle choices. It’s usually a temporary and occasional discomfort.
However, when acid reflux becomes frequent, affecting quality of life and well-being, it’s diagnosed as GERD. Unlike occasional acid reflux, GERD is persistent and indicates a malfunction in the mechanisms that typically prevent stomach acid from flowing back into the esophagus.
Hiatus Hernia and GERD

Hiatus hernia is a condition often diagnosed on endoscopy or barium swallow, result from migration of stomach into chest. Stomach is an abdominal organ, weakening of supportive structures, may lead to migration of stomach into chest, a condition known as hiatus hernia. Predominant symptoms of hiatus hernia occur due to reflux of gastric contents into esophagus
Prevalence of GERD in India, How Common is GERD?
The prevalence of these conditions can vary over time and across different regions. According to the Indian consensus on gastroesophageal reflux disease in adults, the prevalence of GERD in India ranges from 7.6% to 30%, being < 10% in most population studies.
Causes of GERD
When we eat or swallow, a circular muscle at the bottom of the food pipe relaxes, allowing food and liquid to enter the stomach. This muscle, known as the Lower Esophageal Sphincter (LES), then closes to prevent the content from flowing back into the esophagus.
In GERD, the LES may not relax or may weaken, causing stomach acid to flow back into the esophagus. When this happens frequently, the esophageal lining get inflamed and ulcerated.
Several Factors Contribute to GERD
Obesity: Excess weight, especially around the abdomen, can put unnecessary pressure on the stomach and LES, interfering with their normal functioning.
Hiatal Hernia: This occurs when the top part of the stomach migrates into the chest through the diaphragm, a muscle that separates the chest and abdominal cavities. This condition predisposes to reflux of acid into esophagus.
Pregnancy: The growing uterus during pregnancy exerts pressure on abdominal organs, including the stomach. Combined with the abdomen’s expansion, this can weaken the muscles in the diaphragm supporting the LES. The hormone relaxin, secreted during pregnancy, may also relax the LES.
Smoking: Tobacco smoke, whether inhaled directly or through second-hand exposure, can relax the LES. Smoking also leads to coughing, increasing abdominal pressure and opening the LES. Chronic coughing and smoking can weaken diaphragm muscles and may lead to a hiatus.

Other Factors: Eating heavy meals late at night and lying down immediately afterwards can allow stomach acid to flow back more easily due to the lack of gravitational assistance. Some foods, like fried, citrus, and spicy items, tend to relax the LES, making it easier for stomach acid to reflux into the esophagus. Certain medications, including aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs), may contribute to GERD symptoms by irritating the esophagus or weakening the LES.
Common Signs and Symptoms of GERD
GERD can cause various signs and symptoms, and their intensity can differ from person to person and at different times.
Heartburn: This is a burning sensation or discomfort that might move from the chest to throat. It often occurs after eating spicy/oily food or when lying down.

Regurgitation: This involves the backflow of stomach contents, including acid or food, into the throat or mouth, leading to a sour or bitter taste.
Dysphagia: It refers to difficulty swallowing or the feeling of food getting stuck in the throat.
Chest Pain: Similar to the pain of a heart attack, GERD-related chest pain needs to be distinguished from cardiac-related chest pain. A thorough clinical history can help identify GERD as the main cause of pain in patients with non-cardiac chest pain.

Chronic Cough: GERD can cause a persistent cough, often accompanied by the sensation of a lump in the throat. This may result from aspiration of acid into lungs.

Sore Throat: Acid reflux can lead to irritation of the throat tissues, causing a sore throat.

Asthma-Like Symptoms: In some cases, GERD can worsen pre-existing respiratory conditions or mimic asthma symptoms.
Excessive Salivation: Spontaneous filling of mouth due to saliva may occur in response to reflux of acid into the esophagus.Worsening Factors for GERD Symptoms
Worsening Factors for GERD Symptoms
GERD symptoms can worsen under certain circumstances:
Night-time or Lying Down: Symptoms may become more noticeable when lying down, especially during sleep. This happens because, in a standing position, gravity protect against reflux of gastric contents back into stomach. Elevating the head of the bed or using pillows to raise the upper body during sleep can help control or reduce this.

After a Large or Fatty Meal: Consuming a big or fatty meal can increase stomach acid production. When pressure in stomach is high due to excess food, it forces open lower esophageal sphincter (LES), a muscular ring that separates the esophagus from the stomach.
After Bending Over: Bending over shortly after eating will increase pressure in stomach leading to backflow of stomach contents into the esophagus. Maintaining an upright position after meals can help prevent or reduce symptoms.
After Smoking or Drinking Alcohol: Both smoking and alcohol consumption can contribute to GERD symptoms. Smoking can relax the LES, allowing stomach acid to flow back into the esophagus. Alcohol can also relax the LES and stimulate acid production. It’s crucial for people with GERD to avoid smoking and limit alcohol intake.
Complications of GERD
Complications of GERD can include:
Esophagitis: Chronic exposure of stomach acid in the esophagus can lead to inflammation, causing symptoms like pain, irritation, and difficulty swallowing. In severe cases, it may result in the formation of sores and ulcers leading to bleeding. Patient may pass red or coffee coloured blood through the mouth, or complain of foul smelling black coloured stools.
Esophageal Stricture: Continuous exposure and inflammation of the lower esophagus due to stomach acid can lead to the formation of scar tissue. This scar tissue may cause the esophagus to narrow, resulting in a condition known as esophageal stricture. This narrowing can make it challenging for the patient to swallow food.
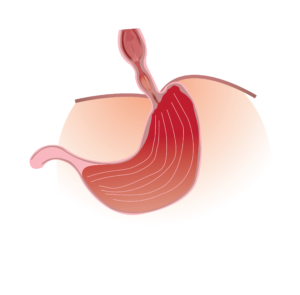
Barrett’s Esophagus: Barrett’s esophagus is a condition where the normal lining of the lower esophagus is replaced by lining of esophagus. This change in tissue type is believed to be a response to chronic exposure to stomach acid. Individuals with Barrett’s esophagus have an increased risk of developing esophageal cancer.
Diagnosis and Treatment
Individuals suffering from heartburn or regurgitation should visit doctor. In presence of classical symptoms, diagnosis of GERD can be made based on clinical symptoms. In patients with persistent or long-standing symptoms further investigations may be required. Following investigations may be helpful in evaluation of patients with symptoms of GERD.
Upper GI endoscopy: During endoscopy, a flexible tube is passed through the mouth into the esophagus and a careful evaluation of food pipe is done. Endoscopy is done after fasting period of 8 hours. It’s better to get endoscopy done during first half of the day. During endoscopy, spray is given remove the pain sensation from throat, intravenous anaesthesia may also be used to have totally painless endoscopy. Ulcer, narrowing or tumor may be seen during endoscopy of GERD patients. Biopsy may be taken from lower esophagus to assist in diagnosis.

24-hour pH study: 24-hour pH study is gold standard for diagnosis of GERD. A thin catheter is passed through nose into food pipe. Catheter has a pH senser, which will detect the amount of acid moving back into the esophagus, measured by a parameter known as Acid exposure time. AET more than 6% is diagnostic of GERD. Acid suppressing medications should be stopped 7 days prior to 24-hour pH study.
Esophageal manometry: Esophageal manometry is a tool to measure pressure of esophagus and lower esophageal sphincter. A thin probe with pressure sensors is passed through nose into food pipe. Esophageal manometry is important tool prior to performing 24-hour pH study or surgery for GERD. It gives information regarding strength of esophageal muscle and can diagnose hiatus hernia.
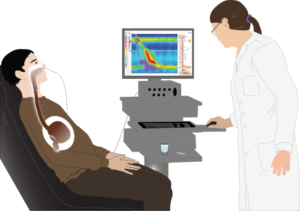
Barium swallow: To determine the most suitable treatment plan for GERD, Barium Swallow test is used. It is a diagnostic test which is used to examine the upper GI tract. During the procedure, patient is asked to swallow a liquid which contains a contrast i.e. barium. Barium helps in highlighting and visualizing the structures of the upper GI tract on X-ray images. As the patient swallows the barium, a doctor is able to observe the size, shape and function of the pharynx and esophagus and will be able to see how the patient actually swallows.
Treatment
- Lifestyle changes: Lifestyle changes are recommended by the doctor as they are considered the fundamental component of the treatment plan for GERD. Avoid trigger foods that may include acidic and spicy foods, chocolate, caffeine, citrus fruits, and fatty or fried foods. Consume small portions of meals that should be consumed throughout the day instead of three large meals. Managing weight if overweight or obese can help reduce the symptoms. While sleeping, raise the upper part of the body with the help of a pillow. If a smoker, avoid smoking as it weakens the LES, making it easier for stomach acid to flow back into the esophagus. These lifestyle changes, when implemented collectively, contribute to a holistic approach to managing GERD symptoms.

- Some medicines like antacids, PPI’s (lower the amount of acid your stomach makes) may be prescribed by the doctor to treat GERD symptoms.
- Endoscopic treatment for GERD: Transoral Incisionless Fundoplication (TIF) is a minimally invasive treatment for GERD. The procedure is performed using an endoscope which is inserted through the mouth and positioned in the esophagus and stomach. The device creates a mechanical anti-reflux valve between the esophagus and stomach by forming folds of tissue held together by clamps. There is no external incision and does not require a prolonged hospital stay.
- Surgery: If the symptoms does not improve with Lifestyle changes and medications, then the doctor may recommend Surgery to treat the same.
- Fundoplication: It is the most common surgical procedure to treat GERD. The doctor wraps the top part of the stomach around the lower esophageal sphincter (LES) to tighten the muscle. This wrapping creates a barrier that helps prevent stomach acid from flowing back into the esophagus, reducing, or eliminating symptoms of gastroesophageal reflux disease (GERD).
- Bariatric Surgery: In case, an overweight or obese patient suffers from GERD, and lifestyle changes and medications have not provided sufficient relief. These patients can go for Gastric bypass surgery.
Conclusion
To prevent the complexities of GERD, awareness, lifestyle adjustments, and timely interventions become key allies. Understanding the nuances of this condition empowers individuals to manage symptoms effectively and promote esophageal health.